ME/CFS and long COVID in Primary Care
ANZMES releases two new resources to guide assessment and management of Myalgic Encephalomyelitis / Chronic Fatigue Syndrome and long COVID.
ANZMES (the national advisory for ME/CFS and a RNZCGP registered provider of continuing education) has released two short reference guides for primary care. These resources offer a snapshot of the key aspects of diagnosis, assessment, symptom management, comorbidities, and care and support planning.
“ME/CFS is a complex and often misunderstood condition, so the aim of this one page resource is to provide a simple reference guide for busy health professionals. We believe that education is key to improving outcomes for patients,” says ANZMES president, Fiona Charlton.
“Although assessment and evaluation for long COVID differs to that of ME/CFS, the management of long COVID, when there is no organ damage, is very similar to the management of ME/CFS. Utilising the expertise of our medical team, we provide a separate one page resource for long COVID in primary care.” she says.
ME/CFS
long COVID
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Definition
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a long-term multi-systemic illness involving the nervous, endocrine, autonomic, and immune systems. The symptoms can range from mild to severe. This guide is designed to help GPs assess and manage ME/CFS and can be used in conjunction with the most current Diagnostic and Management Guidelines for ME/CFS.
Diagnostic Criteria
Despite there being over 20 different types of criteria developed over the past few decades, the criteria produced by the Institute of Medicine, in 2015, is considered the easiest, quickest, and most relevant criteria for a diagnosis of ME/CFS. This stipulates that three primary symptoms must be present: 1) post exertional malaise (PEM) 2) unexplained fatigue 3) unrefreshing sleep. At least one of either orthostatic intolerance or cognitive impairment must also be present. Symptoms must be present for at least six months, be moderate to severe and present 50% of the time.
The symptoms of a number of diseases can mimic ME/CFS, therefore it is important to conduct differential diagnosis to rule out other conditions first (for example,other fatiguing illnesses – anaemia, autoimmune disease, cardiac disease, endocrine disorders, malignancy, rheumatological disorders, neurological disorders – (such as MS, Parkinsons), primary sleep disorder, depression. Routine blood tests and urinalysis will help with this and it is important to note that with ME/CFS these standard tests are often within normal range.
During the acute phase of ME/CFS lymph node palpation may demonstrate slight enlargement. Although this reduces as the illness continues, patients may experience ongoing tenderness and pressure pain points.
Comorbidities
ME/CFS has common comorbidities such as Fibromyalgia (an overlapping condition), dysautonomia, allergies, irritable bowel syndrome (IBS), sleep disorders, Ehlers Danlos Syndrome or hypermobility, and multiple chemical sensitivities (MCS). However the presence of post-exertional malaise and symptom exacerbation, a key illness feature, increases the likelihood of ME/CFS as the correct diagnosis.The NASA Lean Test or the Active Stand Test are useful for diagnosing dysautonomia, such as neurally mediated hypotension or postural orthostatic tachycardia syndrome.
Triggers
ME/CFS has multiple triggers. The virus most associated with this illness is Epstein Barr (mononucleosis/glandular fever), however other viruses (for example, SARS-1, cytomegalovirus) and bacterial infections (for example, lyme, Coxiellia burnetti) are also associated, as are genetics, and environmental factors such as toxic chemical exposure or trauma (physical/emotional). ME/CFS can also be triggered by anaesthesia and surgical procedures.
Symptom Management
ME/CFS is a highly individualised illness, requiring a personalised, patient-centred approach. As there are many symptoms it is useful, in consultation with the patient, to identify the most pressing symptoms and tackle one at a time, per appointment. The main symptoms that can be managed with regular monitoring and review are: pain, sleep, stress, and general health measures. However, the key tool to introduce to patients is pacing – a self-management technique that balances activity and rest to help reduce or prevent PEM. Energy management helps support rehabilitation.
Everyone’s available energy limits are unique and what one person with ME/CFS can do in a day may be very different from another person with ME/CFS. During the course of the illness the energy envelope will fluctuate alongside the severity of symptoms. The more severe the symptoms, the less energy an individual has to do even a basic activity, such as showering or making a meal. In the acute phase, with appropriate pacing, an ME/CFS patient can recover. If symptoms remain longer than 18 months, continued activity pacing is recommended.
Care and Support Planning
Care and support planning is crucial for a patient-centred approach. It is important to assess their individual circumstances and needs and educate the patient on symptoms and prognosis. Empathy is key, and acknowledging the reality of living with ME/CFS can build an effective therapeutic relationship, as can recognising that they may have experienced prejudice or disbelief. It is very important to include written handouts to help counter the cognitive impairments, providing the patient with a summary of your discussion and management plan.Patients may also require work certificates, insurance support, and letters to employers or schools.
When planning care and support a team-centred approach is beneficial, incorporating specialists, physiotherapists, occupational therapists, counsellors, and other health professionals as required. Local ME/CFS support groups can help patients with socialisation, understanding, and support. You can find a list of regional groups on the ANZMES website.
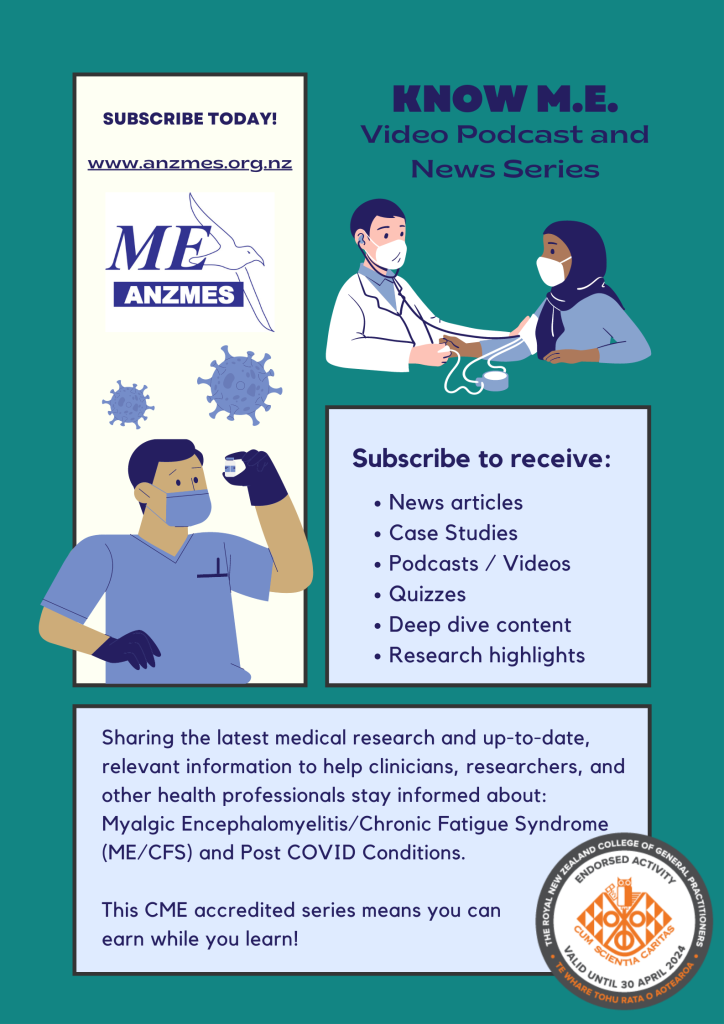
Additional resources with useful information, to inform your clinic practice, include local Health Pathways, the 2021 NICE guidelines,1 and Clinicians Primer.2 ANZMES is currently offering ‘Know M.E.’ – a video podcast and news series, which enables clinicians to earn credits whilst they learn about ME/CFS and post COVID conditions.
References
1 National Institute for Health and Care Excellence.(2022) ‘Myalgic Encephalomyelitis (or Encephalopathy)/Chronic Fatigue Syndrome: Diagnosis andManagement’.
https://www.nice.org.uk/guidance/ng206/resources/myalgic-encephalomyelitis-or-encephalopathychronic-fatigue-syndrome-diagnosis-and-management-pdf-66143718094021
2 Carruthers, B. M. et al. (2012). Myalgic encephalomyelitis: International Consensus Criteria. Journal of Internal Medicine. 270, 327–338.
long COVID
Definition and Trigger
Long COVID has one trigger, the SARS-CoV-2 virus, also known as post-acute sequelae of SARS-CoV-2 or Post COVID condition, or long haul COVID are terms to describe long-term unexplained symptoms following infection with COVID-19 virus and are symptoms characteristic of ME/CFS and post viral syndromes.
Diagnostic Criteria
Long COVID is defined as symptoms consistent with COVID-19 infection that persist for more than 12 weeks after initial infection that cannot be explained by an alternative diagnosis. Symptoms may last weeks, months, or years, and may fluctuate as in ME/CFS. Some people with long COVID, who are still experiencing symptoms after six months, may fit the diagnostic criteria for ME/CFS. The Ministry of Health has published guidelines.
Cormorbidities
As long COVID is relatively new, there is not evidence to suggest that it has typical comorbidities in the way ME/CFS does. It may however, have issues related to organ damage or upper respiratory tract disorders, that are unique to this particular virus.
Symptom Management
People with long COVID experience a wide range of symptoms, with potentially multiple body systems involved, as is the case with ME/CFS. Research is showing that people with long COVID may experience more than 200 different symptoms, and many of them overlap with the experience of people with ME/CFS.
Breathing disorders and upper respiratory tract complications differentiate long COVID from ME/CFS. A referral to a cardio respiratory physio is helpful for breathing pattern assessment.
The cardinal symptom that characterises ME/CFS is post exertional malaise (PEM), which is a worsening of symptoms after physical, mental, or emotional activity, which can occur immediately or up to 72 hours after the activity. People with long COVID are also experiencing PEM or what is more commonly referred to for this subgroup as post exertional symptom exacerbation (PESE). It is very important, despite the patient’s strong desire to return to work, sport, and daily routines, to ensure that they follow a slow, steady, and measured return to activity. Patients must be able to perform daily activities (washing, dressing, meal prep etc) without PESE before a careful, symptom paced return to exercise is considered. An activity diary is very helpful to track symptoms and energy levels, to measure what types of activity induce PESE and those that do not. Referrals to occupational therapists are very helpful for energy saving devices, and support with learning to pace activities.
Care and Support Planning
As with ME/CFS (see information above), a patient-centred approach is paramount. Before a COVID-19 infection, the majority of people experiencing long COVID were healthy, fit, and of working-age, living active lifestyles. The sudden change in functionality and energy can be a big shock and there is much higher incidence of anxiety and depression for people with long COVID when compared to those with ME/CFS. Wellbeingsupport.health.nz is a great resource for free early intervention for mild to moderate mental health support.
The ME/CFS support groups and organisations throughout Aotearoa/NZ have opened their doors to people with long COVID – offering support, advocacy, advice, information, and education.
CME Education
For health professionals wanting to learn more about ME/CFS and long COVID, ANZMES is currently offering ‘Know M.E.’ – a video podcast and news series, which enables clinicians to earn CME/CPD credits whilst they learn about ME/CFS and post COVID conditions.
Visit ANZMES medical professionals page for more information.
ANZMES is the national advisory for ME/CFS offering representation and advocacy, national level support, education, and research funding. ANZMES is a RNZCGP registered provider of continuing education.